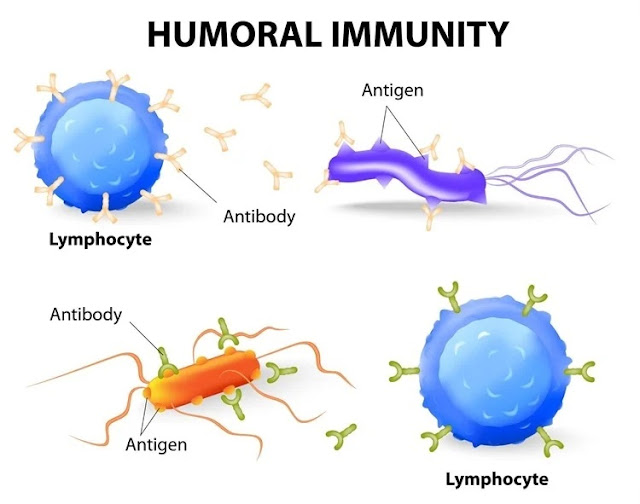
Upon entry of a foreign antigen, macrophages in the lymphoid tissue engulf the antigen and present it to neighboring B-lymphocytes.
Previously dormant antigen-specific B cells immediately enlarge and eventually become plasma cells that secrete antibodies. Plasma cells produce g-globulin antibodies, which are secreted into the lymph and carried in the circulating blood.
Humoral immunity and the Antibodies
The formation of "memory" cells enhances the immune response upon subsequent exposure to the antigen. Some of the B lymphocytes formed after activation of the specific clone do not form plasma cells but instead form new B lymphocytes similar to those of the original clone. This causes an increase in the population for particularly efficient cloning. These B lymphocytes circulate throughout the body and inhabit all lymphoid tissues, but remain immunologically inactive until reactivated by a fresh batch of the same antigen production. Proliferated lymphocyte clone cells are called memory cells. Subsequent exposure to the same antigen leads to a faster and more effective antibody response due to an increase in the number of lymphocytes in a given clone. The increased potency and duration of the secondary response is why vaccination is usually performed by injecting the antigen in multiple doses at intervals of weeks or months between injections. Antibodies are g-globulin proteins called immunoglobulins. All immunoglobulins are made up of combinations of light and heavy polypeptide chains. Every light and heavy chain has a variable part and a constant part. The variable part is different for each specific antibody; it is this part that binds to a specific type of antigen. The constant part determines other properties of the antibody, such as diffusibility, adhesion to tissue structures, and binding to the complement complex. There are five generic antibody classes each with specific features, IgM, IgA, IgG, IgD and IgE. The IgG class contains 75% of most and normal human antibodies.
The antibody attacks an attacker or activates the complementary system and then acts directly to destroy the intruder organism. An antibody can disable the invaside agent directly in one of the following low methods methods:
• Agglutination with a larger particle with an antigen on a surface such as red bacteria or blood cells
• Sol write antigens and antibodies of antibodies too great to be insoluble
• Carrying out the toxicity of antigen agents of the antibody
• Rish (LISI) that can be damaged invasive cells that sometimes attack cell membranes in sometimes cell membranes
Although antibodies have direct impact on the destruction of the invaders, most of the protection provided by the antibody is derived from the amplification effect of the complement system.
The supplementary system is activated by an antigen antigen response. Complement is a collective term used to describe a system of proteins normally present in the plasma that can be activated by the antigenantibody reaction. When an antibody binds with an antigen, a specific reactive site on the constant portion of the antibody becomes uncovered, or activated. This activated antibody site binds directly with the C1 molecule of the complement system, setting in motion a cascade of sequential reactions. When complement is activated, multiple end products are formed. Several of these end products help destroy the invading organism or neutralize a toxin. Supplements stimulate phagocytosis by neutrophils and macrophages, rupture the cell membranes of bacteria or other invasive organisms, enhance accumulation, attack the structure of viruses, reduce neutrophil and macrophage chemotaxis, and enhance macrophages. It may cause the release of histamine by cells and basophils. It enhances the inflammatory process by increasing vasodilation and plasma leakage. Activation of complement by antibody response is called the classical pathway.
Book Update: Pocket Guyton (Twelfth Edition)